In an Ohio hospital system, a physician, William Husel, D.O, is on trial for ordering excessive and fatal doses of fentanyl. He has criminal charges pending against him and he recently pleaded not guilty to murder in 25 deaths. This is the biggest case against an American healthcare professional. (Story and Timeline). The physician ordered potentially fatal doses for 29 patients who died over the past few years. 5 might have had a chance to improve their condition with proper treatment. The defense claims that William Husel, D.O., was alleviating pain and providing comfort for dying patients. However, the fentanyl was 20 times the normal dose which is excessive. And no one questioned them.
Dr. Husel was working a critical, care intensivist at the hospital and he completed a fellowship in critical care but did not complete a required residency in internal medicine according to one source.
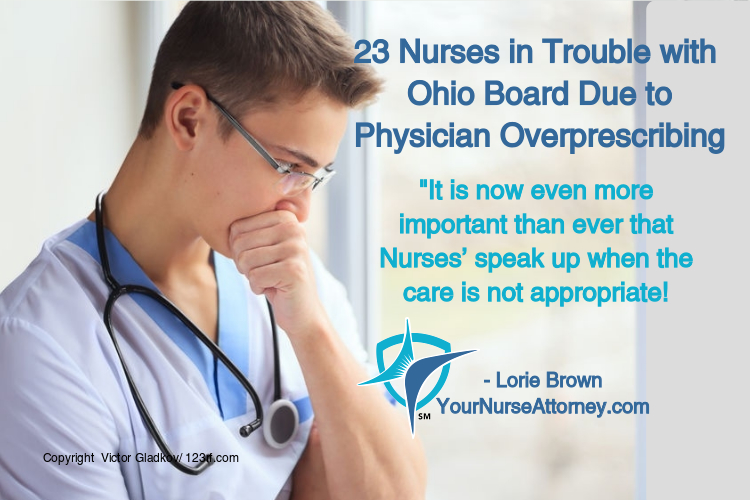
Five (5) managers along with 18 nurses and pharmacists were fired while the CEO of this health system stepped down. (Story). No one ever questioned the excessive doses.
Every nurse has a duty to question doses. Twenty five (25) of these nurses were reported to the Board as well. (Story).
What happened to Hippocratic Oath, physicians do no harm?
There have been several wrongful death lawsuits filed that have reached nearly $4,500,000 in settlement. It is so sad that these families trusted their loved ones to receive appropriate health care but through this doctor’s actions, they were denied.
This case is just an example of the importance of speaking up due to medical malpractice concerns, loss of your job and being reported to the Board. It is now even more important than ever that nurses speak up when the care is not appropriate.
Have you encountered any doctor like this? What would you do? I would love to hear your comments below.




Joan Pate says
I think it’s important that RNs know the medication dose, side effects etc. on EVERY MEDICATION they give b/c they too are held accountable when the dose is outside the normal realm.
After 28 years in leadership positions, I returned to the bedside as a staff nurse in a large, extremely busy Urgent Care Clinic. The MD had ordered Toradol IM; I was familiar with this medication from the inpatient setting where it was given IV piggy back but had never given it IM. So, before returning to the patient’s room, I was reading on the medication and the MD came by the Med Room, asking, “Joan, what’s the hold up with so and so’s Toradol?” I responded that I’d never given Toradol IM and needed to read up on the med before administering it. He looked agast at me and said, “I’ve never seen an RN take that kind of precaution before. You take all the time you need. Can I help you in any way?” I was blown away by his understanding. That’s the good story.
The not so good story are the inexperienced interns and residents who want you to give a med tout suite, regardless of needing to check dosing etc. I recall one incident, where a narcotic was ordered on a post op patient and the dosage was excessive (150mg of Demerol IM) and I was consulting the PDR, when the intern came by and asked what the hold up was. I responded that I needed to check the dosage of the Demerol because it seemed to be excessive. He got mad and told me, to “you need to do what I say and do it now!” I have no use for prima donnas of any type and told him, he could take the syringe and given the injection himself because I was not going to risk my nursing license over a bullying and incompetent physician. I also told him, that as an RN my job was to ensure his prescription agreed with the patient and as a patient advocate I would NEVER give a medication that I thought was harmful. He proceeded to harass me verbally and I told him to leave the unit or I’d have Security remove him. He left the unit, I called the nursing supervisor and informed her of the issue and my actions and requested that she inform the Attending physician that this intern is not welcomed on this floor until I received an apology and change in his behavior. The attending apologized to me the next day and assured me that the intern would behave himself and listen when the RN (who are far more experienced than him) shared about patient care or he would be removed from internship. Just one example of the many negative interactions that have occurred over a 45+ year history as a RN. I’m sure others have similar experiences or worse!
Patricia says
I’ve done the same where I handed the vial to the doc and said, “Well then , you give it!” when I’ve gotten push back when questioning an ordered dose. That usually stops them in their tracks.
But in this case in Ohio, apparently this was an ongoing practice that many complied with and I assume, believed they were “helping” the dying patients along. In some states, it is accepted to give what would be lethal doses for “comfort care” in those dying. Is that what they were defending?