No one ever has become a nurse so that they can sit to document all the care they provided to their patients. Yet, documentation is one of the most important parts of our practice. As much as any of you may dislike documentation, it serves a very important purpose to protect your license and your livelihood as well as protecting you if a medical malpractice claim should arise.
One thing nurses seldom realize is that when they late chart or enter something in a record which is not timed, an attorney can get what is called “audit trails” to find the time that the entry actually was entered into the computer.
Tom Dillow, an informatics nurse and legal nurse consultant in Indianapolis, told me of a female patient on a medical surgical unit who coded in the early afternoon and ultimately died. No rhythm strips were available from the code and, despite being on house wide telemetry, no rhythm strips were documented since the day prior to the code.
The records showed that the patient was in normal sinus rhythm shortly prior to the code, however, the attorneys were able to find that was placed in the chart 31 hours after the patient’s demise. An audit trail was able to determine that fact.
A late entry does raise suspicion, but it must be done properly rather than fraudulently. To stick something in the record hours after the care was performed without labeling it as a late entry is fraud. To properly document, a late entry needs to include the date and time when you are documenting the late entry along with the time and date when the activity or assessment occurred.
If the nurse properly documented the late entry 31 hours later that the patient was in normal sinus rhythm, noting the date and time of the documentation and the date and time when she assessed the patient’s EKG as normal sinus rhythm, it still could raise suspicion. At least with the proper late entry, it is not fraud. Even if it’s a fill in the box documentation, you can still add it is a late entry in the narrative portion.
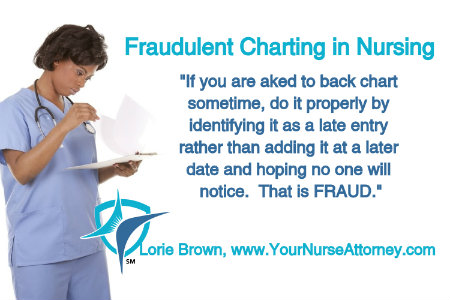
Know your facility’s policies and procedures for late entries. If you are asked to back chart sometime, do it properly by identifying it as a late entry rather than adding it at a later date and hoping no one will notice. That is FRAUD. People forget to document things in the chart but being honest about it with a proper late entry is a lot easier to explain than trying to cover something up.
What are your facility’s policies on late entries? What would you do if your supervisor asked you to “fill in the holes” on a record and not properly identify it as a later entry? I would love to hear your comments below.




Colleen Palmer-Melville says
Thank you Lorie for this very important reminder. As a legal nurse consultant and nursing instructor, I am constantly reminding colleagues and students that honest and accurate documentation is one of the most important aspect of nursing and it is the only thing that they have to show the care that was provided. Lawyers look for every I that was not dotted and every T that was not crossed. Even it had nothing to do with the case, it could be considered.
May says
What is the ramification if ther is no organizational policy that guides late entries?
LORIE A BROWN, R.N., M.N., J.D. says
It there is no facility policy and procedure on late entries, I would advocate for one to protect yourself.
Terri says
Do you know how far back A nurse can add documentation. I was just asked by medical records to chart something on a person left 4 months ago and they want a discharge summary done and I don’t even remember the patient
LORIE A BROWN, R.N., M.N., J.D. says
I don’t think there is a time frame. Check with your facility’s policies and procedures. However, don’t chart anything which you don’t remember. That is fraud.
Cam says
My hospital has been requesting vital signs be documented with in a 30 minute window. When nurses or techs cannot get into the room at that time— say vitals due between 1145-1215 but the tech doesn’t get them until 1pm— management is telling them to back time them and chart them in the window even though they were not taken at that time. But then management doesn’t get in trouble because they are meeting their quotas. So staff is being told to chart vitals 45 mins before they were even taken. I have pointed out that if a bp is 80/40 and you have to complete an intervention then it looks like you did nothing for 45 minutes when in fact that is not the case, the vitals were charted at an incorrect time. If this was discovered what would be the legality of the matter? Can you tell me where the legal guidelines are posted?
Cam says
I was also asked to go back and move vital signs that someone else charted the day before into “the appropriate time window” I told them I didn’t chart them and they asked me to change them anyway. I refused to edit someone else’s charting.
Brenda says
I am not a nurse. I work as an revenue audit clerk. I audit medical records for billable charges. Many charting/charges are missing and I ask the nurses to enter them. If they don’t enter it, I am asked by management to enter them. Some are fill in boxes. Is this fraud? I cant get a straight answer. I dont want to do anything illegal. My job is only to audit. Thanks