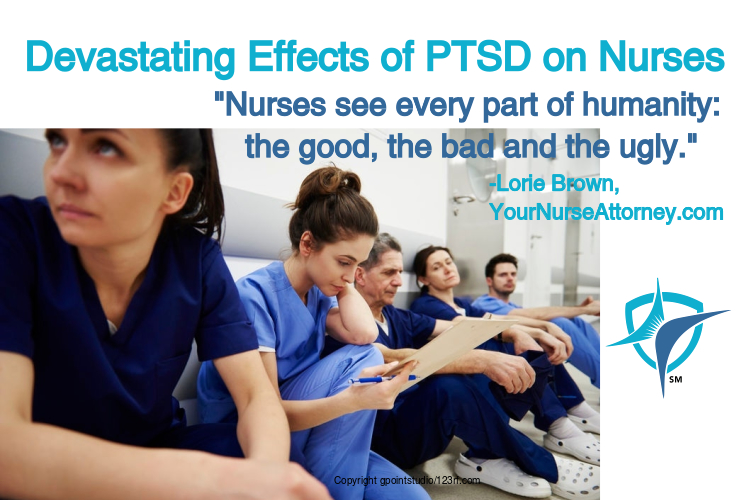
Post Traumatic Stress Disorder (PTSD) occurs in nursing from repeated direct and indirect exposure to traumatic situations. Nurses see every part of humanity: the good, the bad and the ugly.
In a study done prior to the COVID pandemic, 95% of psychiatric nurses in the nation matched the criteria for exposure to PTSD. Another study showed that 24% of ICU and general acute care nurses reported PTSD symptoms as well, while only 17% of emergency room nurses had a probable PTSD diagnosis.
Karen J. Foli, an associate professor at Purdue School of Nursing in Indiana, published an article in April noting that of the 1478 questionnaires, 372 nurses commented about job trauma they had experienced. Responding nurses who work longer shifts and are exposed to unsafe situations that jeopardize patient safety only intensified these findings.
Nurses are required to hurry through tasks, going without food and hydration during their shifts, sometimes without even a restroom break, resulted in unwittingly falsifying patient care documentation. Nurses experienced a range of emotions among which were stress, anxiety, grief, guilt, anger, burnout, and flashback.
According to a February 3rd press release from the University of California at San Diego (USC-San Diego Health), the suicide rates for the nation’s female nurses was 10 out of 100,000 while for male nurses it was 33 per 100,000! This data was compared to the general public counterparts which were 7 out of 100,000 for females and 27 per 100,000 for males.
According to the World Health Organization, suicide is the 10th leading cause of death in the global population. It is so sad that nurses are the forerunners in these studies. Most nurses recover naturally from the mental and physical toll that befalls them, however, a small minority will not.
As a nurse, it is important that you get the help that you need, to work in a safe, supportive workplace and to get early intervention if necessary.
Here are some courses available from nurse.com which can help you understand more about PTSD and anxiety disorder.
In the meantime, if you are not working in an environment that is safe and supportive, maybe you need a change because your mental health and wellbeing are too important, and so is your license. You can always get another job but not another license.




Nurse Undone says
I would caution nurses about discussing this matter with anyone at work or a mgr. You never know who will contact a Board of Nursing. If someone thinks you need counseling , and you do not , they can turn you in to the BON. Some Nurses just go through it with faith or a trusted friend , discussion and time . If the BON agrees you need counseling (and they will) , they can order you to counseling . And if you refuse. The BON can and do charge nurses with violation of NPA , “unprofessional conduct” under “mentally or physically unable to practice nursing ” . If the nurse refuses counseling.
Forced Counseling . Which puts the nurse on probation. So now you are out of income and suffering PTSD. And it is not the counselor who decides when you are “cured” , it is the BON members , who are not qualified . They do this by reading the counseling notes. So a nurse knowing this would not discuss many very private matters and counseling would be ineffective . But they must pay for these visits , and the psychological evaluations , (they will order psych evaluation and a follow up psych evaluation, which the nurse (in az) pays for , not all states charge the nurse, and are costly . The BON can order 12 months probation, but once you sign to agree , they can add 1 -2- 3 years more. You must only go to their “doctor ” who is on their list . But also sign their is no Dr/ Patient relationship , so their license is protected. These Drs are hand picked, and will do what the BON wants ). You must also sign a paper that the BON ‘investigator who may or may not be a nurse, or have any investigative back ground, can have telephone discussions with the psychologist , unrecorded. Yes this does happen , hope this helps someone.