On December 26, 2017, Charlene Murphey was a patient at Vanderbilt Medical Center where she was being treated for a subdural hematoma. A PET scan was ordered and she was transported to that department where she stated she suffered from claustrophobia and was afraid to have the PET scan. Versed was ordered. Why Versed was ordered is unknown without monitoring.
Radonda Vaught, a Tennessee Registered Nurse since 2015 went to the medication dispensary machine to find Versed for the patient. Since the order was not put in the system, the Versed did not pop up on the patient’s profile. Ms. Vaught overrode the system and entered the first 2
30 minutes after the medication was administered, they realized the patient, in the PET scan tube, was not breathing. They resuscitated her but by then she had suffered considerable brain damage and shortly thereafter removed from life-saving equipment.
Nurse Vaught was indicted by a grand jury on January 5, 2018, on charges of reckless homicide and impaired adult abuse
Evidently, Vanderbilt Medical Center swept this matter under the rug and claimed the patient’s death was natural. It was not until a year later, when the Center for Medicaid and Medicare Services (CMS) investigated Vanderbilt and issued its report that the truth of this matter was disclosed and the family was informed.
CMS could have suspended Vanderbilt Medicare reimbursement payments if the hospital did not take steps to prevent future accidents. Vanderbilt quickly provided CMS with a corrective plan so that the reimbursements were no longer in jeopardy.
Surprisingly, Vanderbilt told the Davidson County Medical Examiner that the patient succumbed to a medication error was “hearsay!”
This brings up a couple of issues. First, why was versed ordered without monitoring? And, second, why didn’t a warning pop up on the medication dispensing system about the vecuronium?
Usually cases like this are not just one person’s errors.
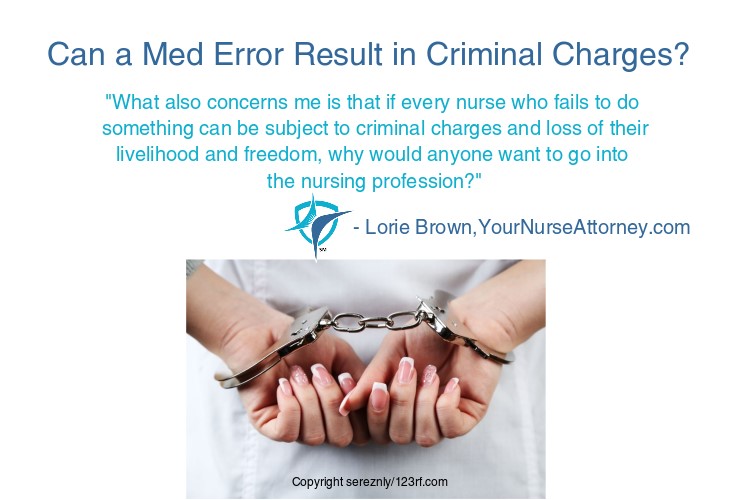
What bothers me is that Nurse Vaught is being charged in a criminal matter. The event was negligence and flat-out malpractice for which the family has not sued. Ms. Vaught clearly violated the Five Rights of Medication Administration and did not note the medication that she was giving.
What also concerns me is that if every nurse who fails to do something can be subject to criminal charges and loss of their livelihood and freedom, why would anyone want to go into the nursing profession?
Obviously, Ms. Vaught was a relatively new nurse and did not have experience with this medication. There is no forgiving her actions but I believe she should not be charged criminally. There was no intent to hurt the patient. Nurse Vaught was just trying to do her job in the best she could.
There 4 elements needed for malpractice. “Duty” which is what those acting under same or similar circumstances would do, “breach of that duty” meaning they didn’t do something they should have done or did something they should not have done, it must cause harm and there must be resultant damages. This is clearly malpractice.
On the other hand, reckless homicide is the killing of another by a reckless act. Reckless means a person acted recklessly with respect to circumstances surrounding the conduct or the result of the conduct where the person is aware of or consciously disregards a substantial and unjustifiable viable risk that the circumstances exist where the result will occur.
Usually, a reckless homicide is when someone recklessly drives another vehicle and unintentionally kills another.
In this case, was Nurse Vaught aware of the substantial and unjustified risk of giving medication and chose to ignore it? That would be for a jury to decide.
I feel sad for her going through this and I hope this does not set a precedent to criminally charge nurses for what should be classified as malpractice.
What are your thoughts are on Nurse Vaught? I’d love to hear your comments below.




Wendie Howland says
If somebody runs a red light and hits a pedestrian in a crosswalk, it’s still a criminal act even if he didn’t mean to kill anybody and feels terrible about it. There were no systemic errors here that prevented a critical care certified registered nurse from performing the most basic check for “right drug” when it was in her hand before she reconstituted it (you don’t reconstitute Versed). She ran that red light. But for that willful act, this woman would not have suffocated. An RN takes responsibility for protecting patients with her first job post licensure and ever after; it is disengenuous to say she wasn’t criminal in so doing when she abrogated her legal responsibility to practice safely.
Joan M. Pate, MS BSN RN-BC says
Another example of a RN who failed to safely advocate for the patient. Several additional problems occurred:
1. Medication had not apparently been ordered in the patient record, so the RN took a “verbal order” which is verboten and risks patient safety. This was not an emergency, so the RN should have contacted the MD to write the order tout suite, before drawing it up & administering.
2. RN was unfamiliar with the med ordered and failed to look up the precautions in giving as well as what sx to watch for, ensuring she was safe following administration. Also unfamiliar with vercromium which is a dangerous med in the best situation.
3. 5 rights were not observed which is a very basic nursing practice and bites the butt every time.
4. RN failed to also recognize that she had a duty to remain with the patient for at least _30 min to ensure no adverse ad developed. Apparently did not do so, most likely b/c of inexperience.
I’ve always approached my nursing practice with a large amount of “what’s in this order (s) that’s going to harm the patient? When there’s something not right with the
order I contact the provider and let them know the problem, and the order will be held until the problem is corrected. Generally, they respond with a lot of verbal abuse, so I respond with, “My job as an RN is to ensure your orders agree with the patient, and this order is unsafe as it is written. ” If you feel so strongly, then come and give yourself, b/c I’m not risking my nursing license.” And I don’t give the med until the problem is corrected.
I started this practice in nursing school b/c. my dad (a med mal atty) & mom (OR RN) were very specific in advocating for patient safety as the RN’s duty is to safeguard the patient from all members of the health care.
Another example of advocacy occured when I was new to a large free standing Urgent Care Clinic (28+ yrs experience) and Toradol IM was ordered. Familiar with med in IVPB form, so was looking it up in the drug book, when the MD came by the med room to see what the delay was. I said I was not familiar with the med in the IM form and needed to look it up! Ready to tell him to give it himself if it was needed asap, but he surprised me, by saying, ” you take all the time you need. It’s such a rarity to hear a RN be so careful in this organization. What can I do to help you?” Took me aback b/ c I’d never received such a supportive comment before.
The moral of the story is never compromise your nursing g practice for ANYONE in any position, because we are held to a standard of nursing practice at all times.
LORIE A BROWN, R.N., M.N., J.D. says
Thanks for sharing! Great moral of the story!